Introducing Bold’s pelvic health program: Improving bladder control, Star Ratings, and member experience for men and women
Pelvic health disorders, including urinary incontinence or bladder control issues and chronic pain, impact up to 75% of women and 21% of men over 65. They are linked to depression and decreased independence, along with costly healthcare episodes including falls. To promote health and well-being for members and drive clinical outcomes for plans, Bold is launching our pelvic health program – the latest comprehensive offering on Bold’s clinical exercise platform.
Bold’s evidence-based pelvic health program means adults 65 and older can access personalized education and exercise classes in a safe, affirming environment. Designed by Doctors of Physical Therapy with pelvic and orthopedic certifications, the Bold pelvic health program helps leading health plans manage costs, reduce falls, and improve their Star Ratings – especially for hard-to-move Health Outcomes Survey (HOS) measures tied to bladder control, falls, and mental health.
“Pelvic pain and incontinence have a high prevalence among aging adults and can greatly impact their quality of life, but due to the sensitivity and stigma surrounding the topic, many individuals are hesitant to seek support or speak with their doctors,” explained Nish Shah, Doctor of Physical Therapy and Clinical Programs Lead at Bold. “Bold’s pelvic health program allows members to learn, exercise, and access care discreetly from the comfort of their home, and is a timely expansion of Bold’s clinical exercise platform building upon our vision of increasing the healthspan of older adults.”
Addressing a common issue shrouded in stigma
Pelvic health is important at any age: the pelvic floor muscles and connective tissues support critical organs in the pelvis, including your bladder, bowel, and reproductive organs. As we age, the tissues supporting the pelvic organs weaken. Overactive pelvic floor muscles or underactive muscles both present issues; the goal for individuals is to find the right balance, which is challenging to determine without guidance from a healthcare provider or physical therapist.
As muscles and tissue weaken or are compromised through injury, pelvic health disorders can arise including:
- Urinary incontinence: loss of bladder control resulting in urine leakage
- Fecal incontinence, resulting in constipation or uncontrolled bowel movements
- Pelvic organ prolapse: the bulging of organs in the pelvis that leads to pain and discomfort
Symptoms like overactive bladder, constipation, incontinence, or pelvic pain are more prevalent than most realize – especially in older adults. Yet despite its prevalence, most seniors aren’t comfortable discussing urinary incontinence or pelvic pain issues with healthcare providers: only 25% to 61% of women who experience weekly bladder control episodes discuss the problem with a provider. This is something that the Centers for Medicare and Medicaid Services (CMS) is actively trying to improve with a dedicated measure for Improving Bladder Control in the Medicare Star Ratings program.
From HOS to costs of care, bladder control is increasingly important for plan leaders
Not only can bladder control issues impact members’ overall physical and mental health and their quality of life, they can greatly impact health plans’ quality measures and bottom lines.
The overall cost burden for individuals with chronic pelvic pain has been estimated at just under $30K for in-network services including treatments, diagnostics, and surgeries – and this is one of the more conservative estimates presented in recent studies.
With the growing importance of annual Star Ratings, Bold’s pelvic health program is designed to improve ratings tied to the following measures:
- Improving bladder control - The measure derived from HOS for Improving Bladder Control has traditionally proven hard for Quality leaders to improve. In fact, the 2025 Star Rating for Improving Bladder Control decreased for the second straight year to 3.0 on average – below the average for Part C measures across HOS, HEDIS, and CAHPS.
- Improving or maintaining mental health - With ties to increased feelings of anxiety, depression, and isolation, urinary incontinence impacts Medicare members’ mental health – which carries growing importance for leaders as the HOS measure for Improving or Maintaining Mental Health will be triple-weighted for 2026.
- Reducing the risk of falling - Urinary incontinence leads to a greater risk of falls: in one study of Medicare claims, those diagnosed with urinary incontinence experienced more than twice as many slips and falls. The HOS measure for Reducing the Risk of Falling performed the worst among all individual Part C measures in the 2025 Star Ratings.
Behind Bold’s pelvic health program
According to the National Institute on Aging (NIA), conservative treatment of pelvic health issues through education and exercise are paramount – in fact, they are first-line recommendations for adults age 65 and older to improve bladder control and reduce pain, incontinence, and other pelvic symptoms. Additional clinical research is building as well: a recent Stanford Medicine-led research study found that women 45 and older who participated in a 12-week low-impact exercise program with yoga, strengthening, or stretching had about 65% fewer episodes of incontinence.
Bold’s evidence-based pelvic health program was designed by Doctors of Physical Therapy with orthopedic and pelvic specialty certifications to specifically support older adults with exercise and education to improve bladder control and address common conditions like urinary incontinence or pelvic pain.
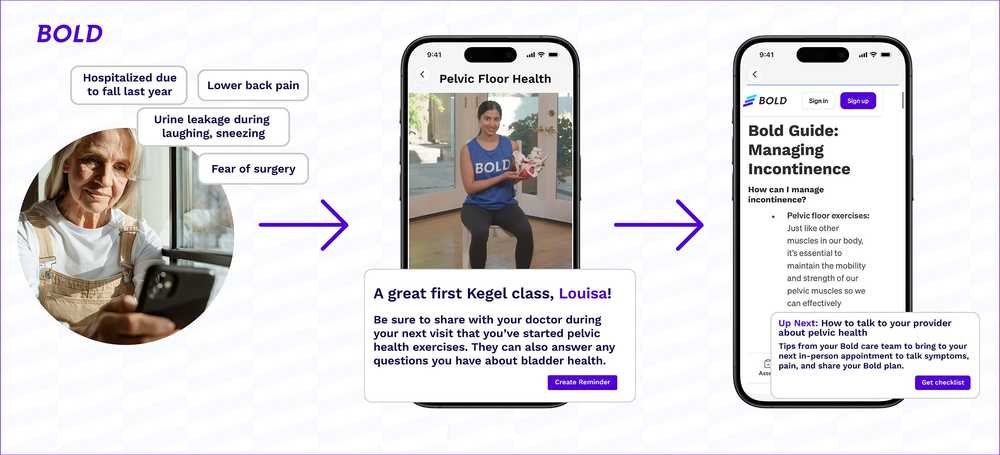
Our comprehensive pelvic health program includes:
- Tailored offerings for unique pelvic health needs, with programs for overactive and underactive pelvic muscles, gender-specific programs, and programs that address general pelvic health, incontinence, or pain
- Pelvic-specific clinical exercise classes taught by Bold Pelvic Health Physical Therapists including diaphragmatic breathing, kegels, integrated practice, and pelvic strengthening moves, to name a few – all with attention to form and guided modifications
- Variety of Bold exercise classes that support and improve pelvic well-being based on the latest clinical practice guidelines, including Balance, Pilates, Strength, and Yoga
- In-depth education content including virtual “Bold Talks” featuring Bold’s Pelvic Health Physiotherapist and Urologist sharing information for members on relevant topics about managing symptoms and preventative care for bladder control, along with Member Guides and Articles on topics like urinary incontinence, how to talk to your provider about bladder control or leakage issues, and why exercise is important for managing bladder control
- Engagement touchpoints and recommended healthy actions for program participants at key milestones to gather self-reported outcomes and collect regular feedback aligned with HOS measures. These include email and in-app notifications that encourage members to take Bold classes or attend “Bold Talks”, complete check-in assessments, read new articles with practical tips and insights, and set reminders to talk to their providers
- Fully virtual programs mean Bold members will have access to exercise, education, and treatment all from the comfort of their own home, which is especially critical for driving engagement and adherence related to bladder control
With the pelvic health program, Bold expands upon our commitment to driving clinical outcomes through our exercise-as-engagement platform. We will capture and continuously measure key outcomes to enable reporting on the program’s effectiveness with Bold’s health plan partners, including statistically significant reductions in pelvic symptoms such as pain and episodes of incontinence.
Aligned with Bold’s clinically rigorous approach, the pelvic health program follows the latest scientific research from clinical practice guidelines (CPG) for pelvic health therapy, including from the American Physical Therapy Association, American College of Obstetricians and Gynecologists (ACOG), and American Urological Association (AUA).
Personalized, virtual program combines clinical exercise and education to drive outcomes
At Bold, we know the power of evidence-based exercise programs purpose-built for Medicare members to deliver value, drive engagement and outcomes, improve independence and longevity, and lower costs of care. More than 9 in 10 members say something they learned from Bold has helped in their day-to-day life. Bold’s pelvic health program integrates with a member’s overall exercise program on Bold and promotes provider engagement.
Ready to learn more about Bold’s pelvic health program? Get in touch to find out what sets Bold apart with clinical exercise for Medicare members.